With the widespread impact of the SARS-CoV-2, understanding all possible routes of viral entry is essential to contain the transmission and spread of the virus. Currently, aerosol transmission via the nasal route is most widely studied and understood; however, the ocular route (via the eyes) has also been suggested as a vulnerable point of entry. In this paper, the researchers investigate the possibility of viral entry via the ocular route using two human-relevant model systems:
Figure 1: Ocular tissues and COVID-19 infection: The ocular tissues have the machinery (ACE2 and TMPRRS2 expression) for the COVID-19 infection and limbus tissue is most prone to SARS-CoV-2 viral replication.
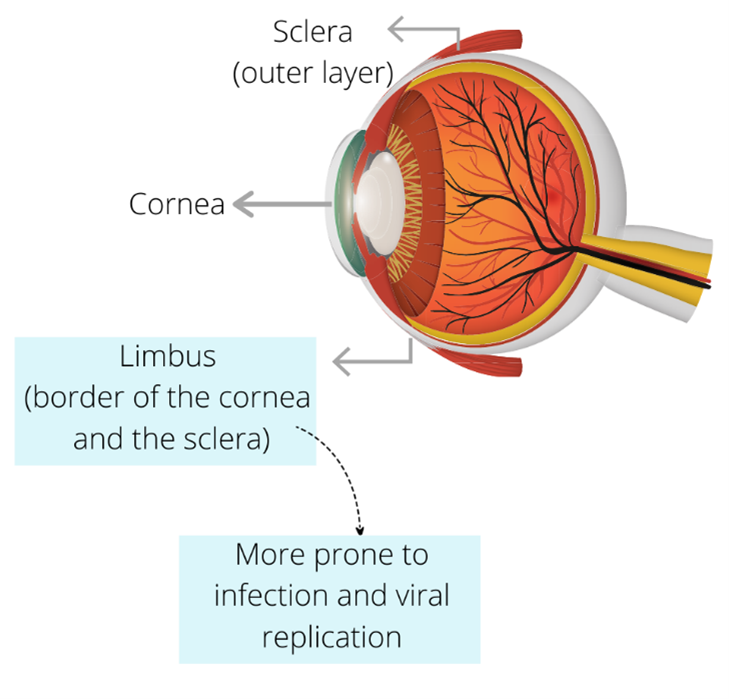
The researchers used these systems to show that SARS-CoV-2 viral antigens are present in the ocular epithelium of COVID-19 infected patients. In addition, the eye organoids could get infected with the SARS-CoV-2 virus when challenged and also generate a NF-kB mediated immune response. Interestingly, they found that limbus tissue (the border of the cornea and the sclera) seems to be most at risk for viral entry because of higher expression of ACE2, TMPRSS2, and other SARS-CoV-2- associated genes. This tissue also has a higher infection propensity compared with other ocular cell types.
The current evidence surrounding COVID-19 infection via the eyes of patients is mixed. A recent meta-analysis of around 895 articles suggested that approximately one out of ten COVID-19 patients show at least one ocular symptom and around 1-5% of COVID-19 patients present the virus in tears. This study presents the evidence that the eye, and particularly the limbus tissue, has the machinery to get infected in an experimental setting.
However, one of the limitations of the study stated by the authors is that it may be difficult to distinguish if the ocular tissue derived from cadavers were directly infected by aerosol droplets or the infection was originally an airway infection which then systematically spread to the ocular surface.
None-the-less these model systems derived directly from human tissues present very powerful models to study SARS-CoV-2 infection dynamics and screen compounds for infection prevention.
Reference: Eriksen et al., SARS-CoV-2 infects human adult donor eyes and hESC-derived ocular epithelium, Cell Stem Cell (2021), https://doi.org/10.1016/j.stem.2021.04.028